Pandemic provides no rest for the weary
Three nurses find their work satisfying despite significant toll COVID-19 has taken on their home lives, overall health
Sophie Leung-Lieu
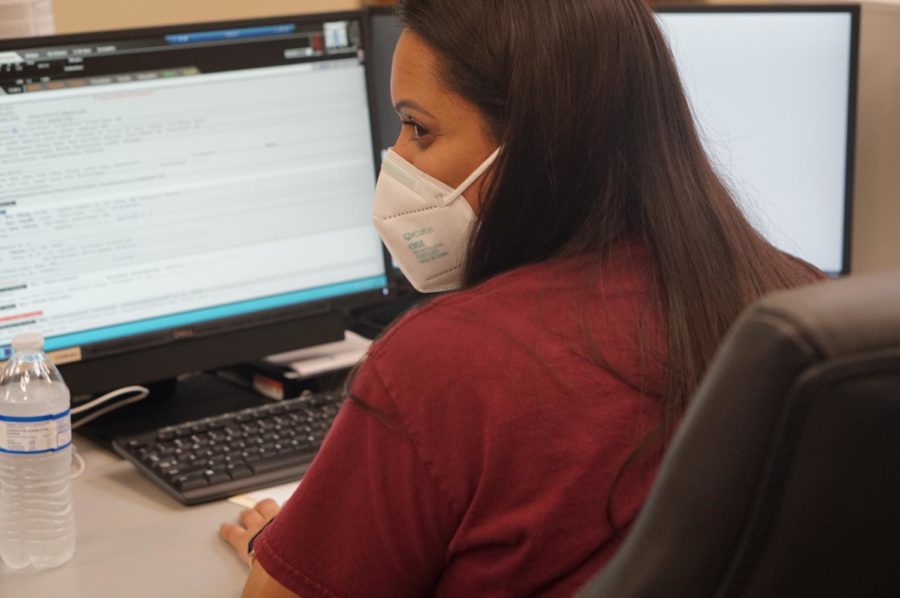
Facility nursing manager Candice Pleasant works as a supervisor to faculty, nursing staff and more. At the start of COVID, emergency facilities had to adapt to the lack of access to ICU. “We have to transfer them or we have to do a video consultation,” Pleasant said. “Not only do we not have those resources, we don’t even have them at our disposal anymore. It’s hard to even get in touch with those doctors. It’s hard to transfer patients. We are left to not only be their advocate, but to be every single person’s specialty for that patient.”
September 17, 2021
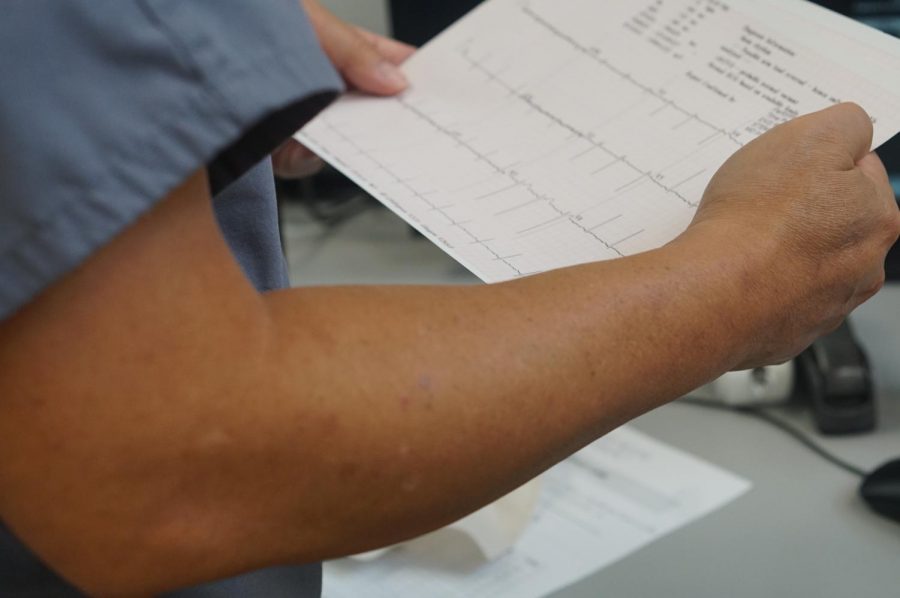
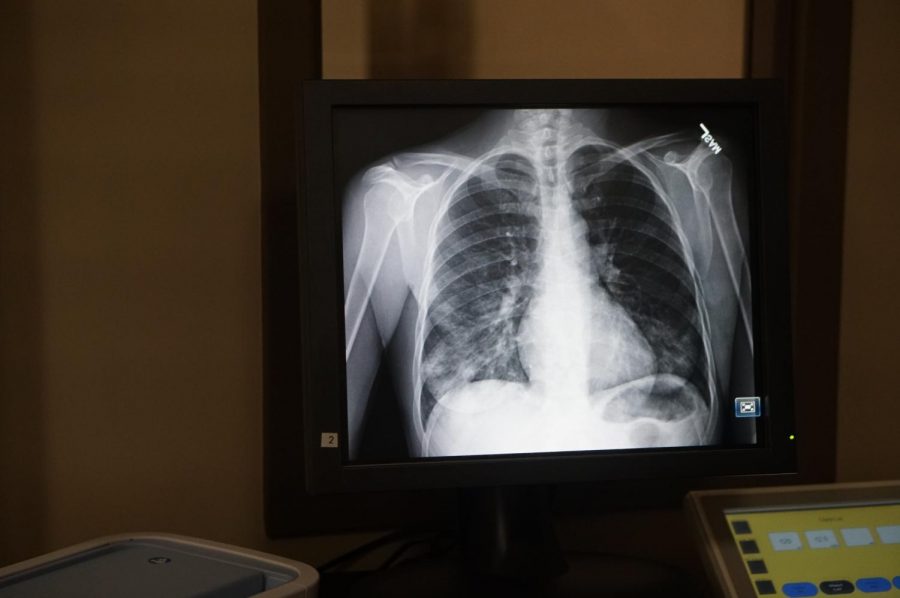
Since the pandemic, working in the medical field has become more rigorous, pressure-filled and detrimental to one’s health. Pre-COVID, Emergency departments saw 50-100 patients per day. Now, they are seeing anywhere between two to three times the pre-COVID daily volume. Because of the influx of patients, some of them with complex illnesses and many that are COVID positive, pressures in the medical field have increased significantly.
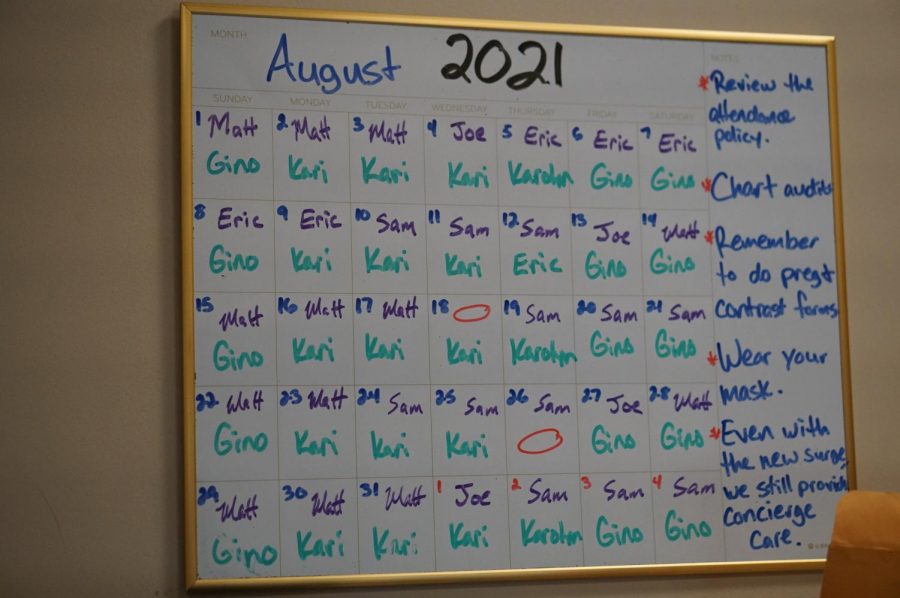
In the early stages of COVID-19, hospital workers took extra precautions to keep their families safe. This included taking off their clothing at the door, showering before touching anything, and cleaning phones, watches, and wallets. Now, almost one year and 250 days later, hospital workers continue to take these extra steps every work day to keep the virus from infecting their families.
But the discipline required to maintain this regimen had done more than just disrupt daily routines. It has also taken a heavy toll on the mental health of medical workers. Since most hospitals never close, most health-care workers operate in 12-hour shifts, leaving them tired and out of energy. Those health-care workers who are also parents with children at home have found it difficult to perform both jobs well during the pandemic. The need for medical workers to work longer hours due to the pandemic has taken away family time at home.
Registered nurse and faculty nursing manager Candice Pleasant works at a 24-hour emergency department. Pleasant is a mother of a young daughter and works 30-40 hours each week beyond her scheduled 40 hours per week. She sees her daughter in the mornings to prepare her for school and typically doesn’t see her again for the rest of the day.
“It’s really hard to maintain the balance right now,” Pleasant said. “I have missed out on so much. … I have guilt because I don’t want to leave the team stranded, and lead by example but you also have that regret that you’re missing out on your kid’s life, and you’re not giving them their full attention, and it’s really hard to be pulled in two different directions.” she said.
Amy Welch, a veteran emergency room nurse of 28 years, has been on duty as a nurse throughout the pandemic and as a result has also experienced strain on her family life. Her daughter, Madison Welch is also a healthcare worker and just graduated nursing school in June 2020.
Madison is currently working at a surgical trauma ICU (intensive care unit) and is working on the frontlines alongside her mom. Although the mother-daughter duo work in separate hospitals, they still share their love of working in the medical field.
Part of the reason that Madison Welch began her career in the medical field was inspiration from her mother. She will return home to tell her mother about her day, and they can both relate on the love they have for the field.
“She is such a good guide in my life,” Madison said. “I thought she was so strong and powerful, and once I began my own experiences, I grew my own passion.”
Amy marvels at the fact that her daughter developed that passion knowing from observation how demanding the job is.
“She has been with me since I have been a nurse so she has seen the blood, sweat, and tears,” Amy said. “For her to still want to go into the medical field because she has seen the love and passion I have for it is just amazing.”
Madison has been in an orientation at Baylor-Scott & White since June 7. Welch is under supervision by a preceptor, who will advise her until she is ready to work on her own.
“There was a period of grace, that was just warming us up to go,” Madison said, “and then we were thrown in.”
Madison is working in the ICU with many experienced trainers and co-workers.
“I have the support of an established person in that field to help me if I need it,” she said.
While Madison has found the work challenging, she’s also found it extremely rewarding.
“Seeing families being able to interact with our patients and seeing the impact it has on their lives, there is nothing better than that feeling,” she said. “All the terrible days, having that experience with the family makes all of it worth it.”
Many of Madison’s patients stay in the ICU for long periods of time, and she loves to see a patient transform into a recovery.
“[The joy] is seeing the progress in their care and them being on a bunch of medications or high ventilator settings and seeing those settings decrease,” she said.
In March 2021, Amy Welch tested positive for COVID. She contracted the virus right around the time that the COVID vaccine became available.
She doesn’t know for certain where she came into contact with virus.
“I could have gotten it at the grocery store,” she said. “Even though you protect yourself 100%; there is always that likelihood that you can get it. Fortunately for me, I was healthy and my symptoms were minimal.”
Even though Madison tested negative for COVID, her mother’s diagnosis made her fearful for many reasons. At the time, Madison was conducting clinicals as a part of nursing school. She took extra precautions at home to stay out of the house as much as possible and to maintain social distancing.
“I wouldn’t want to go to the hospital and get my patients sick.” she said.
Quarantine was a positive experience for many families because it brought family members together. For the Welches, however, it was frightening.
“It is scary that my mom goes to work, and she is around COVID, and I also go to work so it’s scary to think that I could bring that back to my family.” Madison said.
Amid the fear, however, Madison says that the experience did have a silver lining.
“It has brought us closer because we are able to bond over it by talking to each other about what our days are like,” she said.
No matter how challenging the work gets, at least the Welches have each other.
The rest of us may never understand fully how the Welches and Candice Pleasant continue to sacrifice precious family time to continue working in the demanding, changing and taxing environment of pandemic era health care.
But we can hope that they are able to persist until conditions improve, and they are no longer required to sacrifice so much to help the rest of us when we need it the most.
This story was originally published on The Shield Online on September 9, 2021.