While new medical and technological advances aid in the continued growth of the elderly population and the consequent importance of senior care facilities, senior abuse has also become an increasingly prevalent concern.
Senior care facilities, such as assisted living and nursing homes, provide daily care for residents who can no longer care for themselves. Memory care is another option for older adults struggling with cognitive diseases — one in nine people aged 65 years and older show symptoms — that require extra attention.
According to the California Department of Justice, the United States Census Bureau predicted that the state’s elderly population will double to 6.4 million by 2025, the most considerable growth rate in the country.
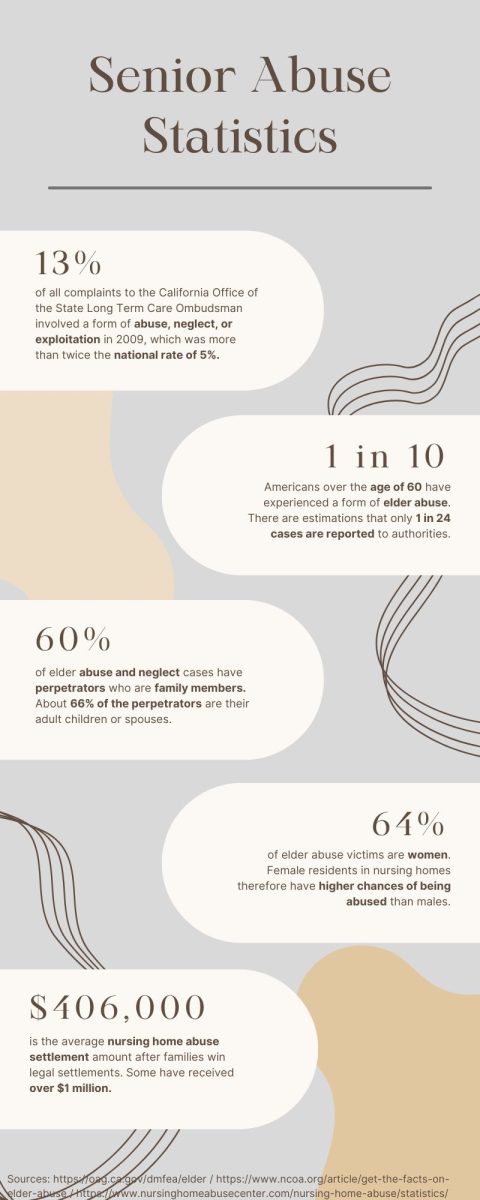
However, according to Nursing Home Abuse Justice, as many as one in three seniors have experienced nursing home abuse. At the same time, around 85% of assisted living facilities have reported cases of abuse or neglect. The World Health Organization predicts that such instances, which increased during the pandemic, are only expected to grow as the world population ages.
Senior or elder abuse can be found in many forms — from emotional or physical to financial or sexual. Annually, hundreds of thousands of adults older than 60 are neglected, abused, or exploited financially, according to the National Institute on Aging.
One factor that can lead to elder abuse in senior care facilities is understaffing: insufficient or inadequate care for each patient. As a result, residents’ physical and mental health can be negatively impacted, and their vulnerability increased.
Ashlee Baker’s story
For Ashlee Baker, whose mother formerly stayed at Oakmont Senior Living in Redwood City, the impacts of senior mistreatment go far beyond the physical.
“My mom had extreme anxiety and panicked behavior after Oakmont. She had lost all sense of physical security because they ignored the residents. People would be wandering around without any interaction because there wasn’t enough staff,” Baker said.
According to Baker, with just a few people on staff, cases where multiple residents would need care left the rest of the residents to their own devices, which could be dangerous.
“My mom is 86 and blind. She had never once had an accident, but I know why she had an accident there. There was nobody around to help her get to the bathroom when she needed it,” Baker said.
While at Oakmont, Baker noticed a lack of care and stimulation for residents, especially those bound to wheelchairs.
“They would park residents in front of the TV and have them sleep for hours on end. Residents were bored, left in their beds, and didn’t get the activities that were promised. There was a decline overall in their physical and mental health because they couldn’t keep their brain active,” Baker said.
It was difficult for her to get in and out of the facility when she visited due to locked doors. Yet Baker still knew of instances where residents accidentally escaped and could have ran out to El Camino Real.
According to Baker, her daughter worked as a hostess at a restaurant and made more per hour than the staff caring for seniors at Oakmont. Because of this wage inequity, it’s hard for the facility to attract decent workers.
“They’re hiring people from McDonald’s and a flower shop. It just doesn’t fly. The people they need to take care of are like newborns. Staff need exceptional patience and understanding because their behavior can make no sense at all. They need to have experience in caring for another human being,” Baker said.
According to Baker, the families at Oakmont believed the care was so insufficient that many had to hire private caregivers to stay by their loved one’s side while at the facility. However, the added costs of a residential home and private aid are often not affordable.
“As soon as your resident can’t feed or can’t dress themselves, they’ll call you and say, ‘We have to up your fee.’ For people that need more care, they somehow justify to them that they need to hire their own private caregivers,” Baker said.
Baker knew some families that were paying over $40,000 a month for complete care — her own family was already struggling with $16,000 per month. She equates the initial charge to renting a room; additional charges were added for care.
As Baker was getting her mother out, one of the staff members in management apologized for her experience before quitting. Baker notes that other staff members at Oakmont worked overtime without the administration monitoring what they were saying or doing.
“They were saying horrible things about family members and residents in Spanish. That was incredibly troubling because these residents cannot tell you what happened to them today or if someone was rough with them. You put so much trust and faith into the fact that these people are caring for your person, so it was really heartbreaking to find that out,” Baker said.
According to Baker, when she visited the facility nearly daily, Oakmont would show good quality of care and good staff behavior, but it didn’t accurately reflect how they treated residents.
“Private caregivers that we hired told us to move our parents. One was so upset by what she witnessed that she had to quit. My mom also kind of told me. I’d say, ‘Mom, did you have breakfast?’ She’d say, ‘I don’t know. I think I did.’ They’d say, ‘Oh yes, Mary, you had eggs.’ But she didn’t have breakfast. They weren’t taking the seriousness of the situation with seriousness at all,” Baker said.
The way Oakmont addressed the COVID-19 outbreak in the facility was Baker’s final straw.
According to Baker, even though the facility knew of staff who had contracted the virus, they were allowed back to work. Soon, many staff and residents were infected as well.
“Every day, someone else would get it, and they never said anything to any of us. Then, one day, I got a call that my mom had a fever. It wasn’t too bad, so I thought, ‘Give her some aspirin and treat the fever.’ The guy says, ‘We’re going to call 911,’ which is what they did when there was anything minor that they didn’t want to deal with. An ambulance ride is about $25,000, and it’s not covered by insurance. I said I would sue them if they took her to the hospital,” Baker said.
Baker lived five minutes away and rushed over with a COVID test to administer for her mom. According to Baker, the employee said they didn’t have any tests when she first suggested testing her mom, and they had no protocol to handle outbreaks.
The same day, another resident tested positive. However, despite the positive test, staff suggested bringing him into the living room, where residents sat side by side. Consequently, most people, including Baker’s family, caught COVID.
After the incident, Baker decided to move her mother out.
“My sister and I got there to move her at 11 in the morning, and she was locked in her room. She had not been fed. She had not gotten changed out of her jammies. She had no care,” Baker said.
Even after they left Oakmont, Baker realized there were aspects of the facility she still didn’t know about.
“We were already out when a private caregiver told us that my mom had escaped the facility. It was scary to think about my blind mom getting out of that facility and onto El Camino,” Baker said.
According to Baker, incidents such as escaping the facility or unexplained bruises from falls were never reported to families despite frequent occurrences.
Oakmont declined to comment.
Christina Galindo’s story
Christina Galindo’s mother is currently a resident at Oakmont. She had loved ones in the same facility when it was under Sunrise Senior Living.
Like Baker, Galindo had to pay for a personal caregiver on top of the $18,000 a month she was paying.
Galindo cares for two people — her mother, who is in assisted living, and a long-time friend, who is in memory care. She has already moved her friend from Sunrise to Gordon Manor, but she and her sister have differing opinions about whether to move their mother.
“My mom is cognitively strong. If you give her the medicine that isn’t hers, she’ll call me and tell me. But when someone’s in memory care, they cannot call you. You have to be there. I was shocked once at Sunrise when I talked to a new employee in memory care who had just graduated from high school, and this was her first job,” Galindo said.
According to Galindo, the staff’s only experience was a 40-hour video training. For Galindo, such training is inadequate for proper care, especially for those with memory issues.
“Memory care people are very, very dependent. Most of them are wheelchair-bound. If you have any experience with a person with Alzheimer’s, you know they get agitated based on fear. To work in memory care, you should be highly trained and know how to handle every situation not only for the residents’ safety but for your own safety, too,” Galindo said.
Galindo developed a contentious relationship with the staff at Sunrise due to what she felt was inexperience and ignorance when dealing with memory care patients.
Galindo hired two very experienced caregivers for her friend, but having them constantly monitor staff as they worked only led to more conflict. Ultimately, she started noticing that essential aspects of care, such as distributing medicine, were not being done correctly.
According to Galindo, each time she would check to see how many pills were left for her friend, the number would not match the projected amount if taken regularly. After working with a geriatric specialist, someone who specializes in caring for older people, she moved her friend out quickly.
“One time, they were dragging a lady by two hands as she was screaming. There are videos of this. Nothing happened to me personally or to my loved one, but I saw things happen, and I reported them,” Galindo said.
The support system of families Galindo had built at Oakmont — which included Baker — helped her through hard times.
“No matter how bad the care is, if you have a good family support system, you can make it better. I always suggest people get to know the other family members. It’s critical. Our system got to the point where when one of us would get sick, the other one would go check on the loved one for them,” Galindo said.
While her loved ones were unlikely to have experienced mistreatment at Sunrise due to her consistent proximity, Galindo still sees a difference at Gordon Manor; she no longer has to check in every day, and her friend is quite happy.
Galindo was shocked to learn that the ombudsmen in California, the people that families go to if they are experiencing mistreatment or a violation of rights, are volunteers.
“It’s ridiculous that it’s not a paid position. There needs to be more of them. When I spoke to an ombudsman, she said she had 13 to 16 different residential facilities to look into. You can’t do that, especially for a volunteer position. They also don’t have any clout,” Galindo said.
Moreover, in multiple instances where Galindo felt that residents were experiencing improper care, licensing never got back to her after she submitted a report.
“One time, I found medication on the floor in five different locations, and I reported it, but licensing never investigated it. Missing medication, especially if it’s a narcotic, should be reported and investigated. When a resident of memory care had gone outside of the facility and was on El Camino, the receptionist who reported it got into trouble because they told her she should have never mentioned it,” Galindo said.
According to Galindo, part of the lack of clout of ombudsmen comes from the fact that, in many cases, no one gets hurt. Their leverage over senior mistreatment investigations mainly comes from an actual incident, not the potential of one.
At Gordon Manor
After moving her mom from Oakmont to Gordon Manor, Baker has noticed significant changes in her behavior and her treatment.
“At Gordon Manor, she’s getting the exercise that was promised. Everyone is brought out to the activities and included,” Baker said.
John Solano is an administrator at Gordon Manor and is in charge of infection control.
When choosing the suitable facility — without worrying about possible abuse — Solano suggests doing extensive research and looking it up on the California Department of Social Services, which shows the number of reports and incidents at each licensed facility.
Gordon Manor is an 82-bed Residential Care Facility for the Elderly (RCFE), with a majority of their residents in memory care, suffering from Alzheimer’s, dementia, or Parkinson’s disease.
The facility provides exercise, music, and interaction to keep residents active.
“We’re trying to provide some quality of life so that people can still emote and have joy. Yes, they get frustrated at times, and they can be anxious. But that’s good. They’re advocating for themselves. That tells me that they’re not happy or they’re in pain. These are all things that help us serve the individual better,” Solano said.
From a caregiver standpoint, Solano values compassion, care, and patience.
The job is also a very mental one, as patients, especially those with mental diseases, tend to have specific needs, such as repeating a question multiple times.
“Emotionally, it can be very exhausting. These older people are moving at their own speed and need to do things in certain ways. If we start to treat people like an assembly line, then it affects their mental and emotional health,” Solano said.
According to Solano, when an older person experiences abuse, they can be traumatized and lose their ability to trust, both now and in the future.
Solano believes the industry has a bad reputation, but not all abuse happens in care facilities.
“Abuse also happens in people’s homes with caregivers or with family members who might not have the resources,” Solano said.
Financial abuse, which may not be as forefront as physical or mental, can also leave lasting damage.
“Sometimes they’re being taken advantage of by an outsider or by a family member who says, ‘I’m just gonna use grandma or dad’s or mom’s credit card to do this because they won’t know,’” Solano said.
Facilities, whether they are corporate or family-owned and operated, can have challenges surviving once a case of abuse occurs.
“Corporate facilities have more resources so that they may reinvent themselves, but it’s tough if you have a family-owned operation and you’re relying on this income to put food on the table. If an outside employee is abusing residents, that has a major impact on your business,” Solano said.
To cultivate a safe space for its residents, Gordon Manor puts a lot of emphasis on the hiring process of caregivers.
“We value the people that are the frontline in this building. The administration is often worried about how we can improve our profit or how we look from the outside, but the caregivers and the nurses are the most important. If you don’t have a solid staff, then it doesn’t matter what your building looks like. It doesn’t matter that you have Stanford or Kaiser on the side of your building,” Solano said.
From the perspective of an ombudsman, caregivers are also a key part of dealing with senior abuse and avoiding it entirely.
“As a person gets older, some falls are unavoidable but can be avoided by having assistance ready. Falls and possible fractures take a huge toll on the elderly because recovery takes so long. They can lose mobility and spiral down very quickly,” said Gail Cameron, a volunteer field ombudsman with Ombudsman Services of San Mateo County.
Senior care facilities are end-of-life care, and patients are mentally and physically declining.
“Dealing with residents who have dementia is beautifully heartbreaking. We have had small victories, but most of them are declining. Sometimes, just a smile or a thank you is so rewarding and gratifying. There are gentlemen who I’ve taken care of personally at the end of life. There are times I’m going home on a Friday and thinking to myself, ‘This is probably the last time I’m going to see them,’” Solano said.
Interaction with residents remains the most gratifying and essential part of care.
“Touch and eye contact really help you recognize what it is to be human. These are people who may not be able to communicate, but you can affect them by sitting with them, holding a hand, or just listening to music together. Shared experience means so much to these people because they’re often confused or anxious. They may not always recognize who I am, but they know I’m there. I’m hoping that they know they can trust me,” Solano said.
This story was originally published on Scot Scoop News on December 13, 2023.