Nausheen Hasan, MHS class of 1997 and medical science liaison, said the rise of opioids around the country is mainly due to their overprescription.
“Pain management is not being handled correctly,” Hasan said. “I think there is a time and a place for opioids, and I don’t believe you should be using it unnecessarily.”
Hasan said fentanyl, oxycodone and oxycontin are opioids that are most often prescribed for various surgical procedures.

“What happens is, after [patients] are fine from their surgery, sometimes they get addicted to it, and want to continue to use it because they perceive they have pain,” Hasan said.
Hasan said to reduce the amount of opioids used, people administering the drugs should be educated, as well as patients, putting a limit on how much substance can be prescribed.
Cai Walz, senior, wants to work at a hospital pharmacy in the future. She said she is concerned about the opioid epidemic plaguing the country. From the pharmaceutical perspective, Walz said it is a tricky situation to decide how to prescribe opioids.
“You don’t want to invalidate their pain or the way they’re feeling, but you also have to gauge if it is an addiction situation,” Walz said.
Walz attended a Cedarville pharmacy camp in 2021 where high school students learned about the basics of prescription drugs. A major topic of discussion was the CDC’s Healthy People 2030 list, which outlines goals for the next 10 years. Walz said the list included the goal of reducing opioid use disorder nationwide.
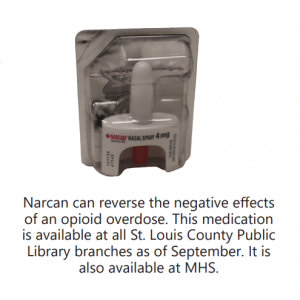
“They taught us that it is important to know how to use Narcan as overdoses are becoming more and more common,” Walz said.
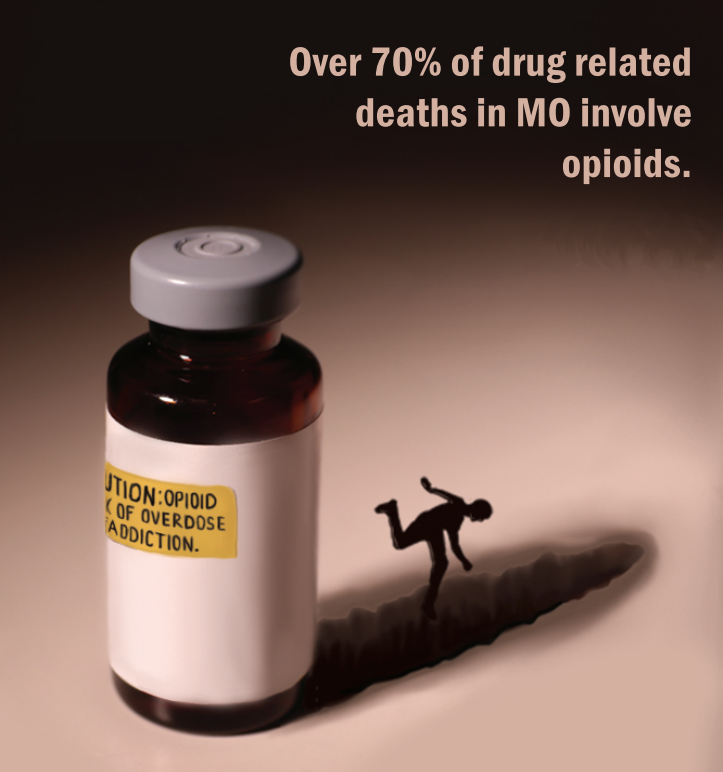
Narcan is the medicine that reverses an opioid overdose, and it was approved for over-the-counter use in 2023. The rate of opioid abuse has been rising in the U.S. since 1999, and more than 1 million people have died due to opioid overdose, according to the Centers for Disease Control and Prevention. The Missouri Department of Health reported 1,424 opioid-related deaths in Missouri in 2022, the highest in state history.
Steve Aspinall, school resource officer, said in the event of an overdose emergency, Narcan is available at the school to combat the effects of opioids.
“The nurse has it, I have one, and I think they are spread out around the school too,” Aspinall said. “I can’t imagine having someone OD and end up dying in the school. That would be horrible, so that is why it is necessary to have it.”
If there were an issue on campus, he said, the nurse would tend to the student and then he would call an ambulance.
Michelle Oertwig, district substance abuse supervisor, handles cases where students are involved with drug abuse. When a student is found abusing substances, Oertwig said the student and their parents go through a series of meetings with district administrators before coming up with a treatment plan.
“They’re suspended 10 days, sometimes more depending on what is said at the meeting,” Oertwig said. “I typically see them within a week or two to go over substance abuse education.”
Oertwig said opioids are currently not a major problem in the district, but students are at risk of abusing drugs that could be laced with opioids.

“If you buy anything off the streets, you’re more likely to buy something that’s laced with maybe fentanyl or other chemicals,” Oertwig said.
Other opioid abuse cases can be linked to post-surgery medication, Oertwig said.
Chase Kuchnicki, freshman running back, tore his ACL last July during drills at football practice. Kuchnicki said he was on painkillers for two weeks following ACL reconstruction surgery, an operation 400,000 people in the U.S. have annually, according to the National Institute of Health.
University of Michigan reports that 1 in 20 young adults use opioids for too long after common surgeries. For Kuchnicki, there was never a concern for addiction.

“It’s pretty much gotten me back to where I was. Before [physical therapy], I couldn’t even bend my knee,” Kuchnicki said. “And it wasn’t hard getting off the painkillers because the pain wasn’t too bad after a couple of weeks.”
Kuchnicki is now six months post-operation and only just days away from finally running again.
Jessi Austin, athletic trainer, said student athletes prone to mental health concerns are at risk for opioid addiction, which is why physicians, therapists and counselors work closely with patients before and after surgery.
“As far as maintaining mental health, that is a huge reason why post-operative patients begin physical therapy early, to give them a sense of community as well as give them tangible goals that they can reach during recovery,” Austin said.
Prescribed painkillers, typically oxycodone, appear in urine drug tests up to four days after consumption and may be used to verify athletes are following their prescriptions. Austin said extra strength Tylenol is a trending alternative treatment option following the first five days post-op.
“There is definitely a risk after surgery,” Austin said. “Avoiding opioid addiction post-surgery sounds like it would be a simple task, but it’s not.”
Health Occupation Students of America (HOSA) hosted an opioid awareness event attended by about 50 students in the Theatre during Ac Lab on March 6.
This event is part of an opioid awareness campaign at MHS organized by HOSA. The club is participating in a community awareness event for their upcoming competition on March 25 and 26, where they will present the findings from their campaign to a panel of judges.
“Our whole goal since September has been to promote opioid use disorder and bring attention to this health crisis,” Zoya Shah, junior, said.
During this Mod, students watched a presentation about the uses of prescription opioids and the effects of addiction. They also learned what to do if someone overdoses on opioids as well as how to prevent overdose.
Shah and Maira Waqar, junior, spoke at the event and are trying to spread information among younger generations. In September, the two began to collaborate with the St. Louis Public Health Department and invited Skyla Barlow, public health coordinator, to speak at MHS.
“I feel like before I started this, I didn’t even know we were in an opioid epidemic, so I hope students take away knowledge and are more careful,” Shah said. “I know in our generation drug use is very common, and it can be really harmful.”
Jessica Hutchings, chemistry teacher, said an opioid is any compound derived from or based around opium found in poppy seeds, and they have specific chemical properties that make them so addictive.
“They bind to receptors in the brain,” Hutchings said. “It is in your mesolimbic system, so the receptors are actually called MU opioid receptors.”
The mesolimbic system is a region of the brain central to dopamine circuits. The release of dopamine, a rewarding chemical, motivates certain behaviors. Hutchings said extended opioid use can cause a tolerance of the drug to form, and it can have long-term effects on the heart, as dependence on artificial painkillers replaces the body’s naturally produced painkillers.

“Because opioids also affect your gastrointestinal tract, you can have bleeding, constipation,” Hutchings said. “People who continuously use opioids have a higher sensitivity to pain, so when they are not taking them, they are extra sensitive to pain.”
Hutchings said opioids can cause different issues in teens versus adults since teen brains are not fully formed yet.
“There is a sheath on those brain cells called a myelin sheath,” Hutchings said. “That layer is not fully formed in the teen brain.”
The positive feelings like euphoria that make opioids addictive are felt more strongly in teens, Hutchings said.
Additional reporting by Morgan Siegel and Samantha Perz.
This story was originally published on Marquette Messenger on March 15, 2024.