Obesity guidelines confront stigma
Matthew McGehee
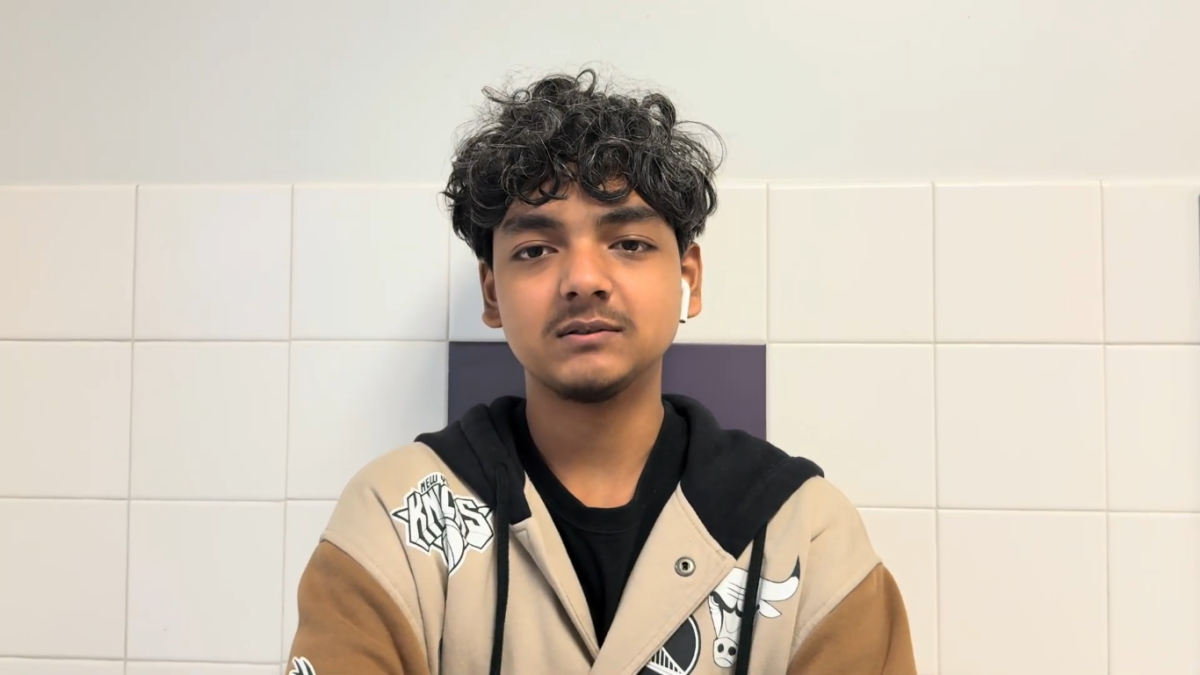
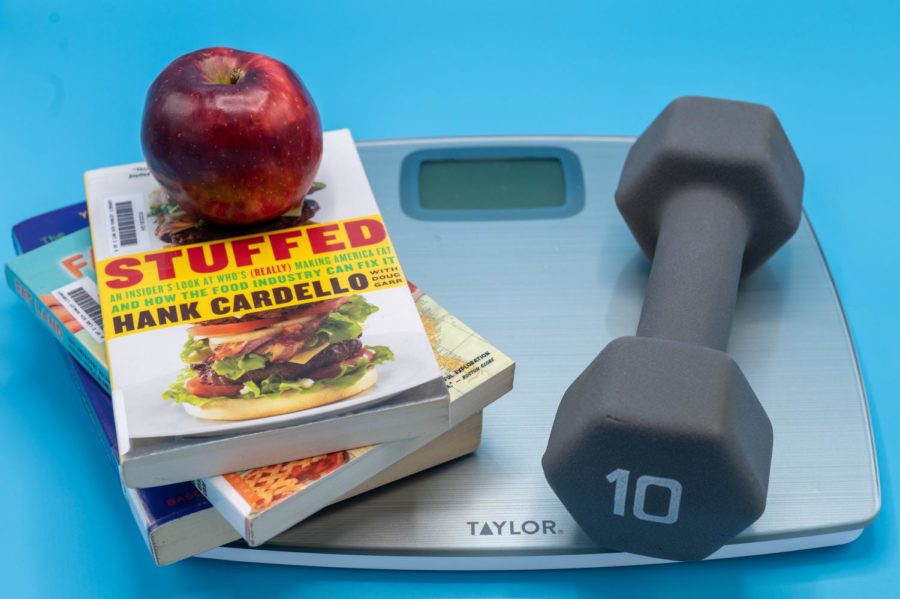
OBSERVING OBESITY. Guidelines from the American Academy of Pediatrics detail the societal stigma surrounding obesity and the many factors that play a role in contributing to the illness, such as family history.
April 10, 2023
Childhood obesity has tripled in the United States, and according to the 2017-2018 National Health and Nutrition Examination Survey, approximately one in five adolescents are affected by this complex disease.
In February, the American Academy of Pediatrics released a 73-page comprehensive report and guideline for the first time in 15 years on obesity in the United States impacting adults and adolescents alike. The guideline confronts the stigma of obesity and the many, sometimes unavoidable, circumstances that create and perpetuate the illness. But it also outlines treatment options ranging from therapy and pharmaceutical prescription to permanent, bariatric surgeries for adolescents.
According to the National Library of Medicine, discrimination toward obese people has significantly increased due to the stigma associated with the disease. A study conducted by the National Opinion Research Center at the University of Chicago showed around three-quarters of the 1,509 adults surveyed believed obesity results from a “lack of willpower” or laziness.
In addition to genetics, according to the guideline and many medical professionals, obesity is caused by many factors, including in-home and community inequities and insecurities, marketing of unhealthy foods, prevalence of racism in obesity and low socioeconomic status.
Jonathan Klein, a professor of pediatrics at the University of Illinois at Chicago, specializes in adolescent medicine and preventive health services, including eating disorders and public health programs. Dr. Klein has reviewed the AAP guideline and agrees with most of the content. He defines obesity as the intake of more calories than you need or that your body uses. However, he also said genetics play a significant role in obesity susceptibility.
“Part of it is the genes that you happen to have been born with, sort of what your amylase tendency is in terms of body happiness,” he said. “Sure, some of it is a function of lifestyle and exercise, but it is clear that a portion of it is really due to biological factors that you can’t change just by exercise.”
The guideline also says the presence of obesity in a person’s family history may affect how they are evaluated and treated.
Dr. Klein said the availability of healthy foods and safe places to exercise, and an obese child’s environment and stress inducers like racism, can prompt obesity much more than eating less and moving more. The guidelines also cover these factors.
“Especially what we find for people living in poverty is that they often don’t have access to healthier foods because they don’t have stores that carry healthier foods, and they might not have the financial resources to be able to buy them,” Dr. Klein said, “so it compounds the problem where you are more likely to be buying things that are at a higher calorie rate and are less gracious in terms of balance to keep your family fed.”
He said it is crucial to view the treatment of obese children as a family-focused intervention rather than a child-focused one.
Dr. Klein said, “Parents decide what gets brought into the house and what gets offered. If you just think about the child as the problem, it doesn’t address the family’s food environment and approach to the availability of healthy food.”
He said part of the solution is helping parents make healthier choices for their whole family.
“It does require having that commitment in implementing a strategy and also the family member’s ability to follow through,” he said. “The parent needs to recognize that they do have some control and opportunity to make different choices, and then help them be able to follow through.”
Dr. Klein recognizes the danger of eating disorders but said that simply discussing food and healthy diets is productive and safe.
“Talking about healthy growth and weight loss doesn’t cause eating disorders alone, but excessive restrictions and struggles over control about food can trigger eating disorders,” he said. “There is a level of caution families should take.”
The guideline discusses how some treatments are more controversial than others.
Dr. Klein views motivational counseling interventions as effective. He said most pediatricians would recommend a lifestyle intervention over a medical procedure, especially for children.
“Surgery is not an unreasonable therapeutic choice for morbidly obese adults and older adolescents,” he said. “However, without being able to make a successful lifestyle intervention, surgery alone is not a magic answer for most people.”
Dr. Klein agrees that stigmatization and negative views toward obesity are problematic. He said he hopes society will shame people less.
He said, “Just because you are larger than somebody else does not make you a bad person, and you can still be quite active in every other aspect of society.”
Body positivity should match personal lifestyle balance
The body positivity movement has encouraged people to have a positive mindset about their body size, shape, and weight regardless of traditional societal standards. But taken too far, living an unhealthy life ignoring weight and possible symptoms of obesity can lead to higher risks of developing diabetes, high blood pressure, asthma and joint problems. So how can people balance accepting their body’s size, shape and weight yet make an active decision to feel good about themselves even if it may mean risking health problems?
Balancing a positive mental mindset around weight with maintaining physical body health can be thought of using weight as only one indication of health, and reshaping the typical language used around obesity.
According to Bethany Hodges, an assistant professor of pediatrics at the University of Chicago, weight is just one of the “vital signs” of health, along with blood pressure, heart rate and oxygenation, so it should be viewed within a larger health context.
For example, a person can be thin but very unhealthy, while someone who is not thin can be healthy if they pursue a healthy diet and physical activity.
However, taking body positivity to the extreme by not paying attention to physical health metrics such as one’s Body Mass Index, or BMI, can create health risks.
Dr. Hodges said a better way to positively address obesity is changing the language surrounding its usage.
“I don’t immediately say something like, ‘You are obese,’ because that sounds negative and judgmental,” she said. “I think it’s a more holistic approach to say, ‘Do you have concerns?’ or ‘How do you feel about your weight and appearance?’ and start from where the person is feeling that they are.”
The body positivity movement confuses Dr. Hodges slightly because it can imply that the default view is a negative body image. She does not want people to think that being overweight is inherently negative, rather it’s more about pursuing a larger healthy lifestyle goals.
“My hope is that you can feel positive about your body regardless of its size and shape.” Dr. Hodges said. “I still want you to feel positive. I just want to help you brainstorm about achieving and maintaining a weight that’s healthy for your body.”
She believes managing obesity as a holistic lifestyle modification can help to destigmatize it. Rather than personal body image being solely focused on weight, other aspects of health can help patients see the broader picture.
Simple tips to help make lifestyle changes include matching screen time with physical activity, eliminating sugary beverages and eating protein with carbohydrates.
Yet Dr. Hodges acknowledges that overall, the body positivity movement helps to address the general stigma of obesity in a way that dissuades unnecessary prejudice.
“I think it’s really important to help educate the public about ways to be supportive for all body types,” Dr. Hodges said, “for the individual person who’s experiencing those things.”
This story was originally published on U-High Midway on April 5, 2023.