President Donald Trump signed into law his “Big Beautiful Bill” on Friday, July 4, carrying spending and tax policies central to Trump’s 2024 agenda. The federal statute imposes a higher endowment tax on multiple universities and limits funding for Medicaid, among other fiscal policies.
Along with cuts to healthcare coverage and education, the bill is anticipated to significantly cut funding to the National Institutes of Health and the Centers for Disease Control and Prevention, along with other research-based public health organizations. Following the funding cuts, the NIH held a hearing to establish its 2026 budget on June 10, emphasizing advancements in areas such as cancer and Alzheimer’s disease research. Jayanta Bhattacharya, the director of NIH, called for an internal review of the organization’s funding allocation, raising concerns about further delays in grants for researchers.
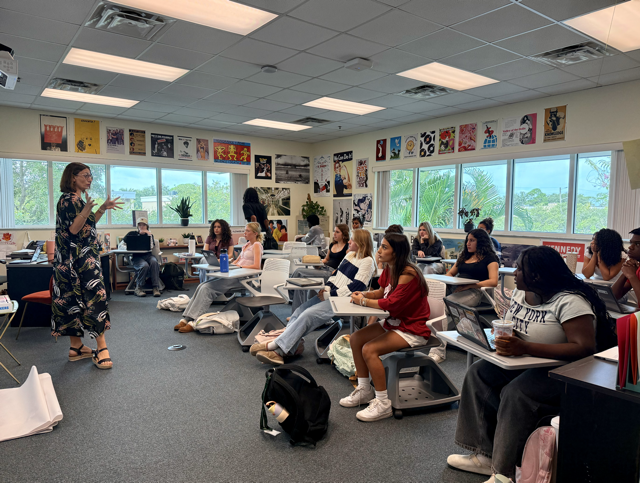
Although Bhattacharya stated in an internal letter to NIH staff that the NIH “continues to support projects across the full spectrum of biomedical research topics,” math teacher Katie Collins believes that limiting resources to medical research institutes will inevitably cause certain unfamiliar diseases and conditions to be overlooked in the coming years. Collins lives with several chronic diseases, including dermatomyositis, a rare autoimmune myopathy that causes inflammation and muscular atrophy. She predicts that autoimmune diseases like dermatomyositis will be among many lesser-known diseases likely to lose research funding in the near future.
“The money is going to be allocated for the most lucrative diseases, which is a term that seems like a contradiction, but medicine is a business now,” Collins said. “Certain conditions like cancer are big moneymakers. So, money begins to be pulled from more rare conditions. Now, no one’s going to fund that research, which means doctors are less likely to go into fields that are not the ones with the most funding.”
Collins’ description of “lucrative diseases” emphasizes conditions for which treatments are extremely expensive, often unnecessarily, so that the profit margin is high for healthcare providers. She explains that some of the services and treatments she has received — for example, intravenous immunoglobulins for her neuropathy — have a markup of 10 or 100 times the medications’ actual cost. If she were uninsured, one IVIG treatment would cost her approximately $50,000. Because of this, Collins emphasizes that women and low-income populations will lose accessible healthcare because of funding cuts to programs like Medicaid and reproductive health services that provide healthcare support to marginalized groups.
Planned Parenthood Mar Monte, the largest planned parenthood affiliate in the U.S., serves the region between mid-California and northern Nevada. On July 24, the organization had to close down five of its Northern California clinics as a result of the One Big Beautiful Bill Act. The law blocks Medicaid funding to nonprofit health clinics that provide abortions, excluding cases of rape, incest or risk to the woman’s life. In response, the Planned Parenthood Federation of America has filed a complaint against the U.S. Department of Health and Human Services as well as the Centers for Medicare and Medicaid Services, alleging that the federal government is retaliating against PPFA due to its advocacy for access to sexual and reproductive health alongside four other allegations.
“Cutting funding to Planned Parenthood is just really an assault on certain groups,” Collins said. “Those federally funded programs provide health care for people who cannot afford it, particularly women, LGBTQ+ people and other minorities, too.”
Collins believes that a decline in accessible healthcare will result in more people attempting to self-treat and self-diagnose, which will significantly impair the health of the current generation. Amit Karkhanis, Director of Strategy at a local healthcare firm, agrees with Collins. He explains that with current Medicaid members losing health insurance, many will forgo seeking healthcare services due to financial struggles. This will ultimately lead to overcrowded hospitals with the neglect of patients’ treatable conditions becoming serious after being allowed to degenerate without proper care.
“For example, I could possibly get admitted to the emergency department due to complications because I just didn’t take care of myself the first time I was sick,” Karkhanis said. “The emergency department is going to be filled with preventable visits because something that could have been rectified by seeing a doctor will eventually become a bigger problem. Getting admitted to the hospital is always expensive to the whole system: the provider and the health plan.”
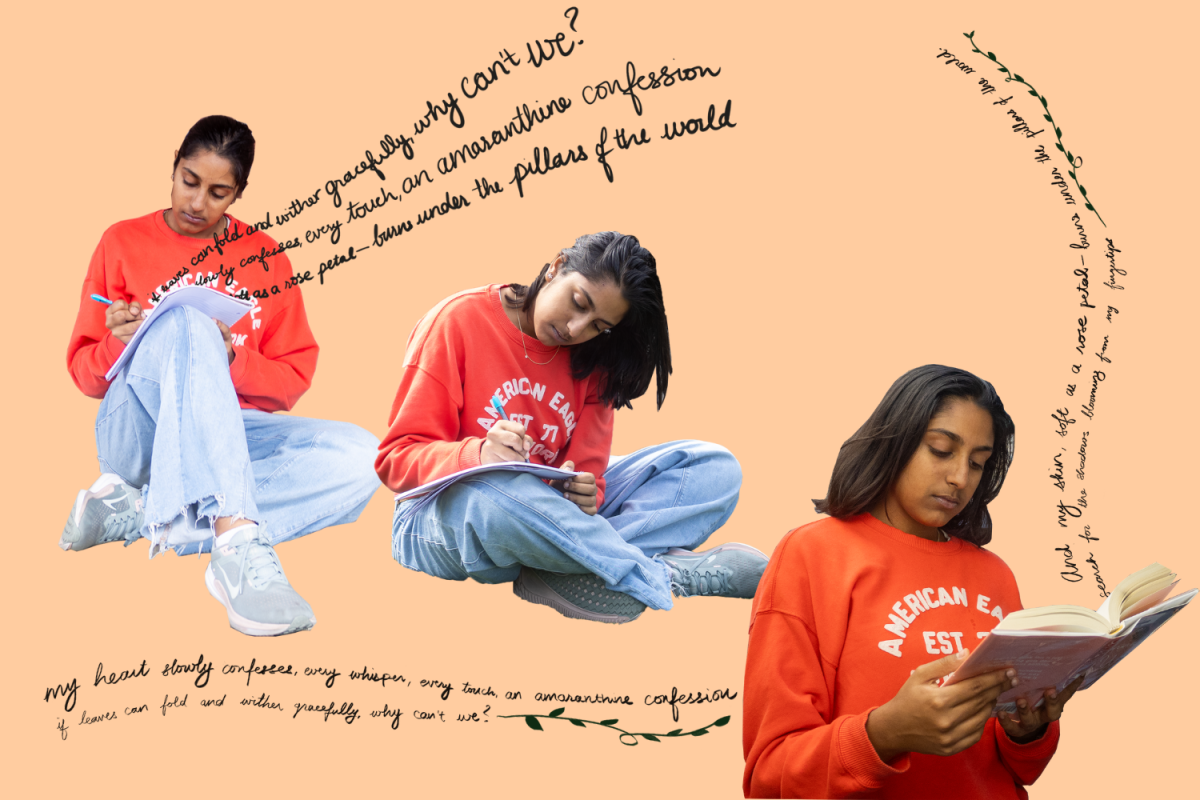
Junior Bhaavya Renukuntla agrees with Karkhanis, looking back on her own experiences of struggling with injuries and other health issues. She acknowledges that from a patient’s perspective, having the emergency department as the only viable option for healthcare is financially unsustainable.
“I cannot stress enough how expensive it was for me,” Renukuntla said. “Even with my parents’ health insurance, the hidden costs of surgeries and ambulance rides was an extremely huge bill to pay. Now, those costs are going to be much worse because of the lack of funding.”
In addition, with the reduction of Medicaid, hospitals will face significant financial losses since hospitals do not receive reimbursement when providing for uninsured patients, potentially impacting how staff choose to provide care. Karkhanis also emphasizes that overfilled hospitals will put a burden on hospital staff, leading to burnout among providers.
“Especially after COVID-19, many physicians, especially in the primary care setting, have left their practices because of burnout,” Karkhanis said. “So if they have more and more members hitting the emergency departments, there’s going to be more burnout. My concern is if we have more hospital staff and providers quitting the healthcare profession, that’s going to be a big problem for the entire health system.”
Collins and Karkhanis both emphasize the real local impacts of these cuts, even as Santa Clara County is one of the most affluent counties in the nation. Statewide restrictions on benefits, provider payments and eligibility requirements would directly impact local communities, especially those who rely on critical healthcare services, inevitably leading to budget restrictions in California overall. However, moving forward, Renukuntla believes state policymakers are responsible for mitigating these effects as best they can to protect citizens’ healthcare access.
“We need to make America a more livable place,” Renukuntla said. “Policymakers should try to not only help get more doctors into hospitals, but also make the cost of healthcare less expensive for people who need it the most, especially in emergency medicine. We need to provide for the people, because that’s what America is supposed to do.”
This story was originally published on El Estoque on October 7, 2025.